The Pharmacist’s Guide to Adjudication: Mastering Pharmacy Claim Rejection Codes and Troubleshooting in Canada
Practical, job-ready guidance for pharmacy technicians and pharmacists working with Canadian adjudication systems, provincial plans, and daily claim troubleshooting.
I. The Foundation of Canadian Pharmacy Billing: Adjudication Explained
When your system sends a claim to an insurer it enters an automated process called adjudication. The adjudicator checks eligibility, formulary rules, and data accuracy. Tiny mismatches — a wrong DIN, incorrect quantity, missing MR code — can cause instant rejections.
A. Understanding the CPhA Pharmacy Claim Standard (CPhAPCS)
The CPhAPCS is the common data format used across Canada. Knowing what fields matter (DIN, quantity, days supply, intervention codes) reduces rejections and speeds processing.
B. The Adjudication Cycle: Submission to Payment
Entry -> electronic submission -> adjudicator checks -> approval or rejection. Each rejection includes a code that points to what must be fixed.
C. The Link Between Billing Errors and Medication Safety (QREs)
Billing errors often mirror safety issues. Many reported medication incidents stem from the same places that cause claim rejections: dose, frequency, quantity. Correct claim handling is therefore a safety step as well as a billing task.
II. Decoding Pharmacy Claim Rejection Codes: Common Reasons

Rejection codes fall into three main groups: eligibility/coverage, drug/formulary issues, and data-entry/system errors.
A. Common Rejection Categories
Eligibility/Coverage: expired plan, limits reached. Drug/Formulary: non-benefit drugs, prior auth needed. Data Entry: wrong DIN, wrong quantity, missing MR code.
B. Detailed Breakdown of High-Friction Rejection Codes
Always reference the insurer’s own rejection list (e.g., provincial plan, Green Shield) to find the exact corrective action. The next section explains common intervention codes to resolve these situations.
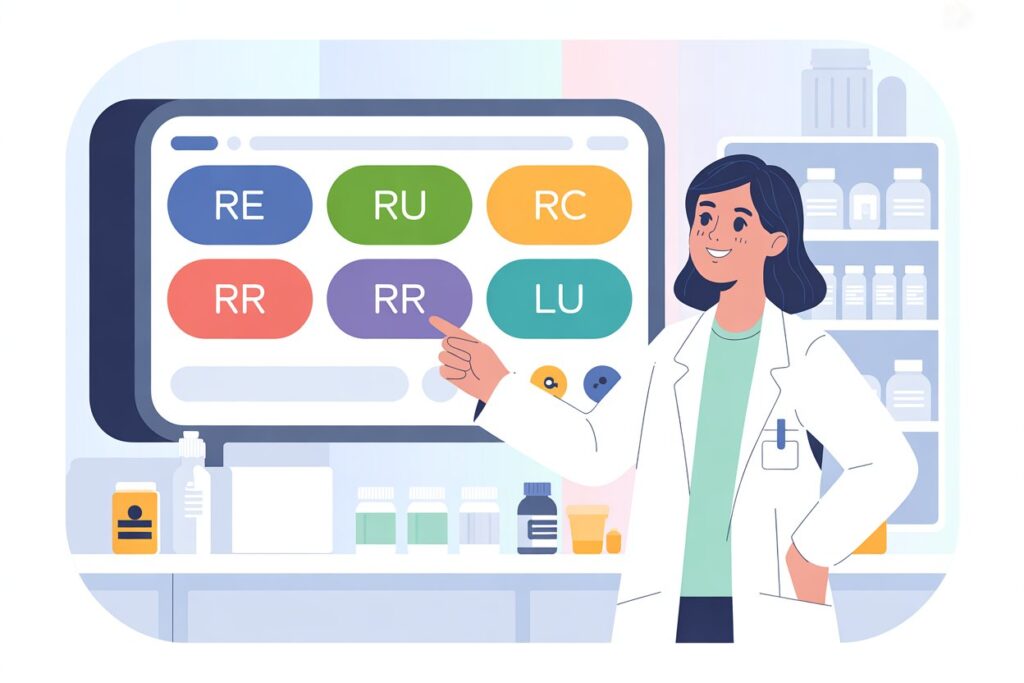
III. Mastering Intervention Codes: Your Toolkit for Claim Resolution
Intervention codes are how the pharmacy responds to a rejection. They document corrections, reversals, or authorizations.
A. The Purpose of Intervention Codes
They speed corrections, support audits, and communicate to adjudicators why a claim was changed or resubmitted.
B. Key Intervention Codes and When to Use Them
| Code | Use Case | Meaning |
|---|---|---|
| RE | Wrong quantity, DIN, or other data entry error | Reverse claim — data entry error |
| RU | Patient did not pick up the medication | Reverse claim — not called for |
| RC | Prescriber cancelled the prescription | Reverse claim — cancelled by prescriber |
| RR | Patient refused medication after dispensing | Reverse claim — refused by patient |
| LU | First-time Limited Use claim (Ontario/ODB) | Start new LU authorization |
IV. Advanced Canadian Billing Scenarios and Troubleshooting
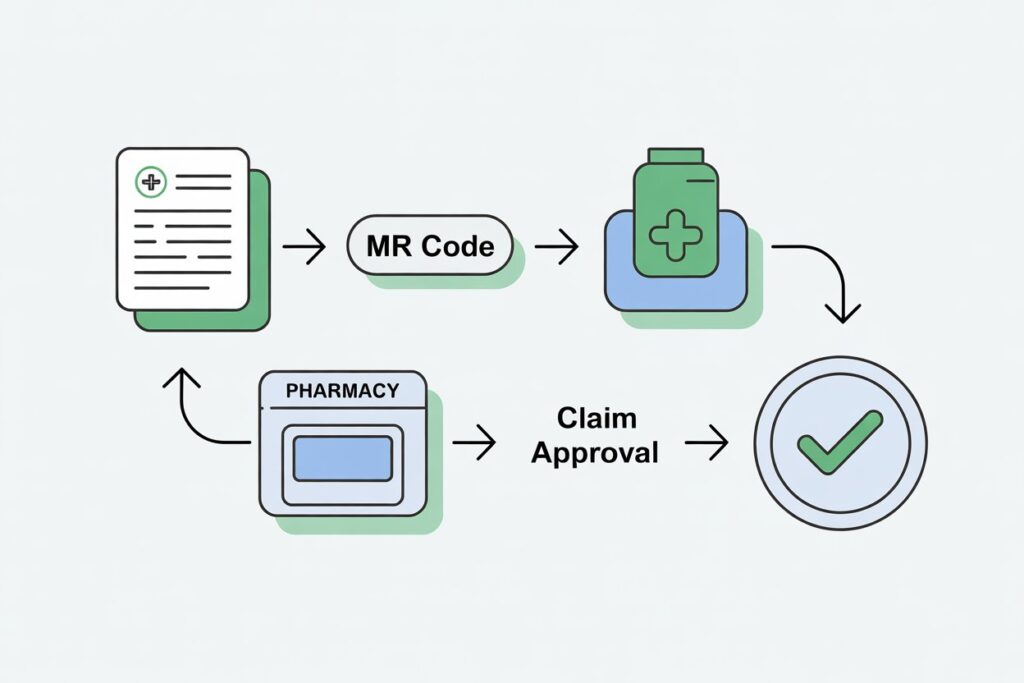
A. Navigating Limited Use (LU) Prescriptions and MR Codes (Ontario)
LU drugs require a prescriber-written three-digit MR code. The LU intervention code is submitted only on the first fill to set the authorization start date. Submitting LU on refills causes rejections.
B. Special Authority (SA) and Non-Benefit Drug Approvals
Special Authority requests allow coverage for otherwise non-benefit drugs. Rejections can be appealed, typically by fax with supporting clinical documentation.
C. Handling Federal Plans (PSHCP) Price Files and Reimbursement
Federal plans use an electronic price file. Paper claims are evaluated against this file, and reimbursements will not exceed the listed price file amount.
V. Systematic Resolution: A Step-by-Step Troubleshooting Guide
A. Step 1: Identify and Document the Rejection Code and Adjudicator
Record the specific rejection code and which plan sent it — this tells you what to fix.
B. Step 2: Determine the Root Cause (Data, Eligibility, or Formulary)
Look for internal data errors first. If everything in your system looks correct, check coverage or prescriber documentation.
C. Step 3: Utilize the Appropriate Intervention Code or Correct Data
Resubmit corrected claims with the right intervention code (e.g., RE for data corrections, LU for initial LU authorization) or call the adjudicator if needed.
D. Step 4: Liaise with Insurers and Adjudicators
For Special Authority or coverage disputes, contact the plan provider. They can often clarify what additional documentation is needed for approval.
VI. FAQs
- What is the CPhA Pharmacy Claim Standard (CPhAPCS)?
- The unified Canadian format for processing electronic prescription claims. It promotes consistency across carriers.
- What is an MR Code and when is it required?
- An MR code is a three-digit code written by the prescriber for Limited Use drugs in plans like Ontario’s ODB to document clinical justification.
- If a PSHCP claim is filed on paper instead of electronically, will the patient be fully reimbursed?
- No. Paper claims are reconciled to the plan’s price file; reimbursement may be reduced to the price file amount.
- What should be done if a Special Authority (SA) request is rejected?
- Appeal the decision with supporting clinical documentation, usually by fax, following the provincial plan’s appeal procedure.
- What’s the difference between an Intervention Code and a Rejection Code?
- A rejection code is returned by the insurer explaining why a claim was denied. An intervention code is entered by the pharmacy to fix or justify the claim.